Authors
Carrie L. Gigray, PhD(c), MSHS, CHSE, CHSOS, NRP1,2,3, Crystel L. Farina, PhD, MSN, RN, CNE, CHSE, ANEF4, Michael D. Hollins, MBA, MPA, MA5, Robin D. Hayes, AS6, Nicole C. Brown, PhD, MSN, RN, CHSE-A7, Shannon K. T. Bailey, PhD8,9
1HealthySimulation.com, Las Vegas, NV
2Washington State University College of Medicine, Spokane, WA
3Providence Health, Spokane, WA
4George Washington University School of Nursing, Ashburn, VA
5University of Nebraska Medical Center, Omaha, NE
6Independence XR Design, Castro Valley, CA
7Cleveland Clinic, Cleveland, OH
8Center for Advanced Medical Learning and Simulation, University of South Florida Health, Tampa, FL
9Morsani College of Medicine, University of South Florda, Tampa FL
Conflict of Interest Statement
The authors of this manuscript declare no conflicts of interest.
Corresponding Author
Carrie L. Gigray, PhD(c), MSHS, CHSE, CHSOS, NRP, HealthySimulation.com, Las Vegas, NV, Washington State University College of Medicine, Spokane, WA, Providence Health, Spokane, WA
(Email: carriegigray@hotmail.com)
Brief Description
Haptic technology, which enables touch sensation, holds significant potential to improve fidelity in healthcare education and practice, especially when combined with extended realities (XR), such as virtual reality (VR) or augmented reality (AR). Sensations, including force, touch, and temperature, may be helpful to simulate clinical tasks such as feeling for a fever, palpating a vein, or other psychomotor skills. This paper explores current and emerging trends of haptic technology in healthcare simulation, the potential for haptics to enhance clinical education and practice, and the need for future research, technology, and investment.
Introduction
One of the primary challenges of utilizing haptic technology in healthcare simulation has been the dearth of codified terminology for understanding, assessing, and categorizing haptic sensations and their implications (Parisi et al., 2019). Definitional imprecision has stagnated scholarship, impeding research investigating capabilities and limiting haptic technology in healthcare simulation. With the maturation of a shared vocabulary for understanding haptic sensations, research into haptic techniques can flourish. Defining haptic terminology will help facilitate further research and development while enabling content creators to more easily integrate haptics into hardware and software solutions for greater effectiveness.
Definitions
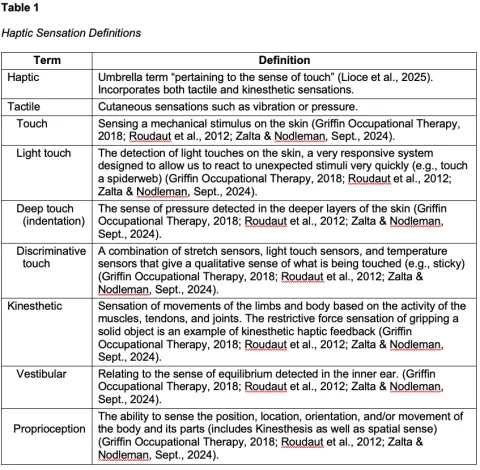
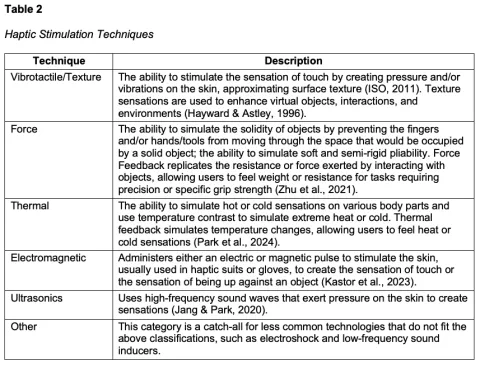
The Society for Simulation in Healthcare defines haptic as “pertaining to the sense of touch” (Lioce et al., 2025), but the term haptic is often used inconsistently. For example, the International Standard Guidance on Tactile and Haptic Interactions uses tactile and haptic interchangeably (ISO, 2011). In contrast, much of the scientific literature treats tactile as a specific type of touch sensation that falls under the broader category of haptic sensation. o promote clarity, the authors propose defining haptic as an umbrella term that includes tactile sensations, such as vibration and pressure, and kinesthetic sensations, such as those produced by receptors in muscles, tendons, and joints that detect movement and tension (Haptics, n.d.). To assist with understanding the definitions and possibilities of haptic feedback, haptic sensations are defined in Table 1, and haptic simulation techniques to achieve different sensation effects are defined in Table 2. These definitions may aid healthcare educators and simulation developers to choose devices that are most aligned with their learning needs.
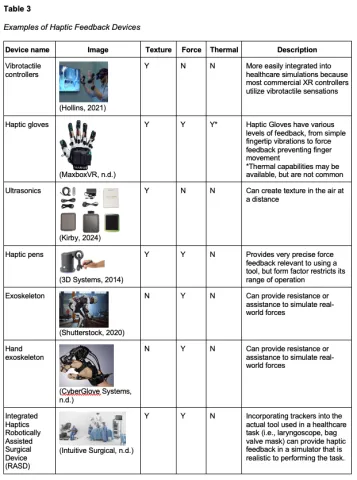
The variability in haptic taxonomy is evident in the numerous ways haptic devices have been categorized, including by form, user interaction, wearability, and underlying technology. Examples of how different simulation techniques are incorporated into various haptic devices can be found in Table 3. Adilkhanov et al. (2022) conducted a literature review that analyzed over 90 haptic devices and subsequently created a taxonomy of haptic devices based on the extent of wearability. They defined three broad categories of devices: grounded (e.g., haptic pens), hand-held (e.g., video game controllers), and wearable (e.g., haptic gloves, exoskeletons). This differs from other reviews which focus on the techniques for providing haptic feedback, such as actuator type (Lelevé et al., 2020). For example, haptic devices may use brakes, which are passive actuators that provide a feeling of force feedback by stopping a user’s hand from moving to simulate a solid object. This differs from pneumatic actuators that use compressed air to create the feeling of force. Although both are categorized as force feedback, the underlying technology differs, each with their own benefits and limitations for implementation into healthcare simulation.
Problems with Technology
Existing literature indicates haptic devices offer various types of tactile and kinesthetic feedback, such as vibrotactile/texture, thermal, force, or a combination of sensations (Alford et al., 2024; Zhu et al., 2024). Examples of haptic technologies and the types of feedback they provide are listed in Tables 2 and 3. Although each technique presents unique challenges, common issues across device type include high cost, bulkiness, interference with movement, high power consumption, and limited adaptability for different users. Tactile feedback, specifically, is challenging to provide complete hand coverage to meet the needs of different healthcare simulation tasks. Kinesthetic feedback also faces challenges balancing bulky, heavy active force mechanisms with lighter, passive actuators. As explained by Alford et al. (2024), emerging technologies such as “liquid metal, transcutaneous nerve stimulation, and air pressure systems,” are in development to enhance haptic feedback quality, but these technologies are not widely available.
In addition to hardware challenges, haptic devices typically rely on specialized software and application programming interfaces that are not commonly included in standard XR development pipelines. As a result, developers and educators integrating haptics into simulations must manually incorporate these tools, which presents a significant challenge for widespread adoption. As described in Alford et al. (2024), “the ideal haptic device would be lightweight, low cost, [user-friendly], and capable of delivering [multiple types of sensory] feedback” that can be utilized across healthcare tasks.
Evidence of Efficacy
Haptic research is growing, as noted by the increase in scholarly publications from 250 in 1995, 4,500 in 2015, 7,200 in 2018, and over 640,000 in 2025 (Parisi et al., 2019). Despite the growing literature on haptics, evaluating the efficacy of haptic devices for healthcare simulation remains challenging. Definitions of haptic devices in training environments vary widely, making it difficult to compare outcomes across studies when the technologies are not consistently described or categorized. At the same time, the tasks trained are highly variable. Haptic devices have been used in healthcare simulation for disparate tasks, including suturing, endoscopy, laparoscopy, palpation, ultrasound, and across specialties such as dentistry, emergency medicine, gynecology, and surgery (Coles et al., 2010; Escobar-Castillejos et al., 2016). Although there are many examples of haptics used in healthcare training, most reviews on the efficacy of haptics in healthcare simulation have focused on surgical simulations (Azher et al., 2024; Mackenzie et al., 2022).
Research on haptics is still nascent, but there are promising examples of haptics in the development of surgical skills. Rodrigues et al. (2022) found that the haptic-enhanced VR system showed high usability scores, indicating that participants found the technology intuitive and efficient, which led to improved surgical precision, confidence, and procedural outcomes in dental surgery training. Haptic feedback has also shown promise in increasing bone drilling efficacy to reduce the risks of neurovascular injury in orthopedic surgeries (Gani et al., 2022). However, literature reviews highlighted the lack of quality evidence to support conclusions on the impact of haptics in healthcare training due to small sample sizes, biased study designs, incomplete reporting practices, and a dearth of evidence on the transfer of training to clinical practice or patient outcomes. The notable conclusions from these reviews and surveys are that there is an urgent need for haptic research in healthcare simulation to standardize research protocols, incorporate larger sample sizes, validate simulators and simulation methods in various contexts and for different learners, and to ultimately measure patient outcomes.
New methods of creating and integrating sensors and actuators, along with innovative feedback strategies, are necessary to address these limitations. The call for the collaborative development of open-source haptic preprogramming underscores the importance of ongoing research and development, which are crucial to realize the full potential of this technology in healthcare education. Haptic devices present the potential for enhancing the sensation of touch during healthcare training, but technical and practical challenges must be resolved. Further research is also essential to understand how and when to best use haptic devices in healthcare simulation.
Future State
Haptics in healthcare education are considered immersion-enhancing tools within XR platforms. The use of haptics augments users’ suspension of disbelief to deepen their connection to the teaching content, which generates increased agency, empathy, understanding, and a heightened sense of involvement. This is significant because increased immersion may lead to improved learning outcomes and retention (Zhang, et. al., 2019). The haptic sensorial layer is so synonymous with all immersive virtual world interactions that experiences without haptic properties may feel inadequate or low fidelity (Söderström et al., 2022). Thus, as XR hardware and software proliferate in terms of accessibility and fidelity, complementary haptic technologies should co-evolve to achieve an analogous breadth and depth of touch experiences in healthcare education.
Following a similar trajectory of integration into personal technologies (phones, vehicles, etc.), healthcare training will domesticate the haptic vocabulary within immersive environments. Additive immersion achieved through novel physical sensation will become the expectation. Just as gamers have come to expect touch as a central component of connection to the virtual world, healthcare practitioners will increasingly demand that haptics be integrated into the overarching simulation experience.
One challenge to advancing adoption of haptics is that development of hardware for XR use is extremely time- and cost-intensive. At times, this development can require exorbitant budgets and multi-year development cycles to launch iterations of previous models. Likewise, XR software development involves an investment of time and resources that must be justified through a valid return on investment. In lieu of compelling evidence that the initial investment in haptic technology is offset by an increase in the efficacy of an XR experience, healthcare educators often decide to utilize a simulation modality with known outcomes. Without a universal language for understanding haptic experiences and research to illustrate its impact, healthcare haptic technology will not achieve significant industry penetration in training or patient care.
Research evaluates results, results designate impact, and impact stimulates investment. Thus, a growing body of research around haptics in healthcare training and patient care outcomes will eventually yield results in terms of applications that create the best outcomes. This, in turn, will further technology investment and enrich the canvas of possibilities for haptic development. XR platforms will standardize the realm of possibility for enhanced immersion with haptics, which will further refine content creators' tool sets and processes for meaningful integration.
Recommendations for Future Research and Development:
- Research is needed to establish the efficacy of haptic devices for specific clinical tasks, with careful attention to functional-task alignment (Hamstra et al., 2014).
- Studies should clarify the educational value added by haptic devices compared to existing technologies, such as high-fidelity manikins.
- Because different parameters of haptic fidelity may require varying levels of implementation, research should identify the degree of haptic feedback necessary to achieve specific learning outcomes.
- Cost–benefit analyses, such as those described by Foo et al. (2020), are essential to determine whether the educational gains of haptic devices justify their investment.
- Interdisciplinary collaborations among researchers, clinicians, and developers are necessary to evaluate device capabilities and limitations while informing industry of educational needs.
- Healthcare simulation content incorporating haptics is currently limited, and there is a need for more simulation content incorporating haptics across a wider range of clinical domains.
- Future development of haptic devices should prioritize affordability and accessibility to enable broad adoption across training programs.
Conclusion
Haptic technology has the potential to improve healthcare simulations; however, current limitations must be addressed to facilitate broader adoption. Standardized terminology will ensure that haptic technology groups work effectively with other collaborators in education, research, and development. Healthcare simulation professionals need to standardize terminology and frameworks to successfully integrate haptics. Unified standards for haptics between healthcare and industry can enable platform interoperability across sectors and enhance the accessibility of content creation. The future of haptics in healthcare simulation lies in overcoming these obstacles through the continued advancement of hardware, software, and interface design, which will lead to more immersive, adaptable, and effective educational tools. Further research is essential to address current challenges and fully harness haptics to meet the complex evolving needs of healthcare education.
References
3D Systems. (2014). 3D design you can touch [photograph]. https://www.barcodesinc.com/media/pdf/3D-Systems/touch-3d-stylus.pdf
Adilkhanov, A., Rubagotti, M., & Kappassov, Z. (2022). Haptic devices: Wearability-based taxonomy and literature review. IEEE Access, 10, 91923–91947. https://doi.org/10.1109/access.2022.3202986
Alford, N., Moffitt, S., Okuda,Y., & Bailey, S. K. T. (2024). Wearable haptic feedback devices in virtual reality for healthcare simulation training: A narrative review [Poster Presentation]. International Meeting on Simulation in Healthcare (IMSH), San Diego, CA.
Azher, S., Mills, A., He, J., Hyjazie, T., Tokuno, J., Quaiattini, A., & Harley, J. M. (2024). Findings favor haptics feedback in virtual simulation surgical education: An updated systematic and scoping review. Surgical Innovation, 31(3), 331–341. https://doi.org/10.1177/15533506241238263
Coles, T. R., Meglan, D., & John, N. W. (2010). The role of haptics in medical training simulators: A survey of the state of the art. IEEE Transactions on Haptics, 4(1), 51–66. https://doi.org/10.1109/toh.2010.19
CyberGlove Systems. (n.d.). CyberGrasp [photograph]. https://www.cyberglovesystems.com/cybergrasp#photos
Escobar-Castillejos, D., Noguez, J., Neri, L., Magana, A., & Benes, B. (2016). A review of simulators with haptic devices for medical training. Journal of Medical Systems, 40(4). https://doi.org/10.1007/s10916-016-0459-8
Foo, J., Cook, D. A., Tolsgaard, M., Rivers, G., Cleland, J., Walsh, K., Abdalla, M. E., You, Y., Ilic, D., Golub, R., Levin, H., & Maloney, S. (2020). How to conduct cost and value analyses in health professions education: AMEE Guide No. 139. Medical Teacher, 43(9), 984–998. https://doi.org/10.1080/0142159x.2020.1838466
Gani, A., Pickering, O., Ellis, C., Sabri, O., & Pucher, P. (2022). Impact of haptic feedback on surgical training outcomes: A randomised controlled trial of haptic versus non-haptic immersive virtual reality training. Annals of Medicine and Surgery, 83. https://doi.org/10.1016/j.amsu.2022.104734
Griffin Occupational Therapy. (2018). Everything You Need to Know About the Touch Sense – Griffin Occupational Therapy. Retrieved from: https://www.griffinot.com/touch-sense-sensory-processing
Haptics. (n.d.). In Merriam-Webster Dictionary. https://www.merriam-webster.com/dictionary/haptics
Hamstra, S. J., Brydges, R., Hatala, R., Zendejas, B., & Cook, D. A. (2014). Reconsidering fidelity in simulation-based training. Academic Medicine, 89(3), 387–392. https://doi.org/10.1097/acm.0000000000000130
Hayward, V., & Astley, O. R. (1996). Performance measures for haptic interfaces. In Springer eBooks (pp. 195–206). https://doi.org/10.1007/978-1-4471-1021-7_22
Hollins, M. (2021). Vibrotactile controllers in educational demonstration. [Photograph]. Personal collection.
International Organization for Standardization (ISO) (2021). Ergonomics of human-system interaction: Framework for tactile and haptic interactions. ISO Standard No. 9241-910. https://www.iso.org/obp/ui/#iso:std:iso:9241:-910:ed-1:v1:en
Intuitive Surgical. (n.d). DaVinci SP surgical system operating room set up [Photograph]. Intuitive Surgical Press Resources. https://www.intuitive.com/en-us/about-us/newsroom/press-resources
Jang, J. & Park, J. (2020). SPH fluid tactile rendering for ultrasonic mid-air haptics. IEEE Transactions on Haptics, 13(1).
Kastor, N., Dandu, B., Bassari, V., Reardon, G., & Visell, Y. (2023). Ferrofluid electromagnetic actuators for high-fidelity haptic feedback. Sensors and Actuators a Physical, 355, 114252. https://doi.org/10.1016/j.sna.2023.114252
Kirby, D. (2024). How does Ultraleap’s mid-air haptics technology work? Ultraleap for Developers, 8. https://support.ultraleap.com/hc/en-us/articles/360004377257-How-does-Ultraleap-s-mid-air-haptics-technology-work
Lioce, L., Lopreiato, J., Anderson, M., Deutsch, E., Downing, D., Robertson, J., Diaz, D., & Spain, A. (2025). The terminology and concepts working group, Healthcare Simulation Dictionary (3rd ed.), Agency for Healthcare Research and Quality. https://www.ahrq.gov/patient-safety/resources/simulation/terms.html
Lelevé, A., McDaniel, T., & Rossa, C. (2020). Haptic training simulation. Frontiers in Virtual Reality, 1. https://doi.org/10.3389/frvir.2020.00003
Mackenzie, C. F., Harris, T. E., Shipper, A. G., Elster, E., & Bowyer, M. W. (2022). Virtual reality and haptic interfaces for civilian and military open trauma surgery training: A systematic review. Injury, 53(11), 3575–3585. https://doi.org/10.1016/j.injury.2022.08.003
MaxboxVR. (n.d.). Quantum gloves by Manus [photograph]. https://www.maxboxvr.com/shop/product/quantum-gloves-by-manus/
Park, W., Korres, G., Jamil, M. H., & Eid, M. (2024). Neural correlates of thermal stimulation during active touch. Frontiers in Neuroscience, 17. https://doi.org/10.3389/fnins.2023.1320417
Parisi, G. I., Kemker, R., Part, J. L., Kanan, C., & Wermter, S. (2019). Continual lifelong learning with neural networks: A review. Neural Networks, 113, 54–71. https://doi.org/10.1016/j.neunet.2019.01.012
Rodrigues, P., Esteves, A., Botelho, J., Machado, V., Zagalo, C., Zorzal, E. R., Mendes, J. J., & Lopes, D. S. (2022). Usability, acceptance, and educational usefulness study of a new haptic operative dentistry virtual reality simulator. Computer Methods and Programs in Biomedicine, 221, 106831. https://doi.org/10.1016/j.cmpb.2022.106831
Roudaut, Y., Lonigro, A., Coste, B., Hao, J., Delmas, P., & Crest, M. (2012). Touch sense. Channels, 6(4), 234–245. https://doi.org/10.4161/chan.22213
Shutterstock. (2020). Black African American engineer testing futuristic[photograph]. Shutterstock https://www.shutterstock.com/image-photo/black-african-american-engineer-testing-futuristic-1870469299
Söderström, U., Larsson, W., Lundqvist, M., Norberg, O., Andersson, M., & Mejtoft, T. (2022). Haptic feedback in first person shooter video games. In ECCE 2022: Proceedings of the 33rd European Conference on Cognitive Ergonomics, 24, 1-6. https://doi.org/10.1145/3552327.3552333
Zalta, E.N., & Nodelman, U. (2025) Stanford Encyclopedia of Philosophy. https://plato.stanford.edu/
Zhang, L., Bowman, D.A., & Jones, C.N. (2019). Exploring effects of interactivity on learning in interactive storytelling in immersive virtual reality. In 2019th 11th International Conference on Virtual Worlds and Games for Serious Applications, VS-Games, 1-8. https://doi.org/10.1109/VS-Games.2019.8864531
Zhu, J., Yang, B., Song, A., Liu, K., Sun, D., & Tang, Z. (2024). Review: The development of tactile feedback devices. Ninth International Symposium on Sensor, Mechatronics, and Automation System, 1298134, 1-7. https://doi.org/10.1117/12.3014791
Zhu, Q., Du, J., Shi, Y., & Wei, P. (2021). Neurobehavioral assessment of force feedback simulation in industrial robotic teleoperation. Automation in Construction, 126, 103674. https://doi.org/10.1016/j.autcon.2021.103674