Authors
Jason Konzelmann, M.Ed., CHSE, CHSOS, FSSH1, Jacob Givoni, BA1, Mason Criswell, BA1
1College of Medicine, University of Central Florida, Orlando, FL
Conflict of Interest Statement
The authors of this manuscript declare no conflict of interest.
Corresponding Author
Jason Konzelmann, M.Ed., CHSE, CHSOS, FSSH, Clinical Skills and Simulation Center, College of Medicine, University of Central Florida, Orlando, FL
(Email: pamedic848@gmail.com)
Abstract
Incision and drainage of skin abscesses is a common yet essential medical procedure that requires hands-on training. Ethical concerns around practicing on live patients highlight the need for effective simulation models. However, current commercial trainers are often costly and lack realism. We developed a low-cost, high-fidelity abscess trainer using DragonSkin™ silicone molded in a 6-well escargot tray to create realistic abscess wheals filled with food-grade materials to simulate pus. The trainer features multiple sites, enhancing skill development and cost-efficiency. Medical students and residents evaluated the trainer’s fidelity across key procedural steps: anesthetization, incision, drainage, packing, and dressing. Learners reported high satisfaction with the model's anatomic realism and stepwise procedural accuracy. Comfort performing the procedure improved from a mean of 3.9 to 4.6 on a 5-point Likert scale (1 = highly uncomfortable, 5 = highly comfortable) after training. Participants strongly recommended continued use of the model for teaching this skill with a mean score of 4.6 on a 5-point Likert scale (1 = highly unlikely, 5 = highly likely). This novel trainer offers a realistic, reusable, and inexpensive solution for teaching skin abscess incision and drainage, with appropriate fidelity for all steps in the process.
Introduction
Simulation practice and training have shown to be useful and effective (Gordon et al., 2016), giving participants the opportunity to practice skills without risking harm to real patients (Sagalowsky et al., 2016). It also enables them to practice, receive feedback and practice again in rapid succession to improve competency quickly (Singh & Restivo, 2024). Procedural trainers are needed to fill a gap in surgical and procedural training that can otherwise be ethically challenging when practiced on real patients (Thyagarajan et al., 2024). Incising and draining abscesses are essential skills in many healthcare specialties (Nicka & Swanson-Biearman, 2019).
Commercially available task trainers for abscess incision and drainage (I&D) are limited, are often expensive, and have myriad drawbacks. A recent internet search revealed models range from $42 for a pack of six to over $170 for a single-incision device. Some commercial trainers require refrigeration to prevent spoilage, while others contain latex risking severe allergic reaction in sensitive participants. Others lack visual and procedural fidelity elements, only allowing for certain steps in the overall I&D process or are only available in one skin color. Commercial trainers also take time to order and deliver.
Available literature describes homemade models, each with their own set of drawbacks (Chambers et al., 2024). Heiner (2010) inserted simulated abscesses into cadaverous chicken breasts for later incision, drainage, and removal of the cystic casing. Since it contains raw meat, it requires refrigeration, has a short shelf life, meaning it cannot be made long before the training session, and carries inherent risk of salmonella poisoning (Heiner, 2010). It also has a limited number of purulent sites since it requires a valid location in the chicken breast to insert a balloon (Heiner, 2010). Several other models describe a similar preparation with a balloon and food-grade products that have varying degrees of realism and shelf life or require cadaverous tissue for implantation of the abscess (Done et al., 2020).
This novel training model is low cost and free of the limitations previously described. Our model costs approximately $7 per pad with six independent abscesses, or a little over $1 per abscess, allowing for procedural repetition. The pad can be made in as little as 4 hours. It does not require refrigeration, animal or human tissue, and is not perishable. The trainer possesses an extended shelf life up to 6 months and can be constructed with any desired skin tone.
This paper aims to evaluate if our novel training model is effective at replicating key aspects of skin abscess I&D with medical students and residents who have varying experience performing I&D. Participants can practice all steps in the process including circumferential anesthetization, incision, pus expression and complete drainage, and packing the empty wound (Pastorino & Tavarez, 2024). We predict this trainer demonstrates high procedural fidelity, indicating suitability for training any level of learner. We hypothesize that participants will recommend it for future trainings.
Methods
Model Design
A custom, low-cost abscess I&D trainer was created using three types of Platinum CureTM silicone: DragonSkin™ 10 Very Fast, Eco-flex™ Gel, and Eco-flex™ 00-30 Fast silicone rubber (Reynolds Advanced Materials, n.d.). Simulated pus made from food grade mustard and mayonnaise replicates tactile and procedural fidelity of abscess management. It was evaluated by medical students and residents during one of two structured skills workshops. All materials used are listed in Table 1. The authors encourage visiting https://www.reynoldsam.com/product-category for further information on each of the products described; however, it should be noted that the authors do not endorse one product brand over another.
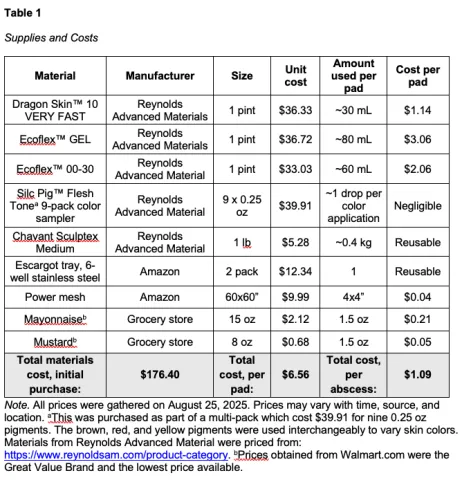
Note. All prices were gathered on August 25, 2025. Prices may vary with time, source, and location. aThis was purchased as part of a multi-pack which cost $39.91 for nine 0.25 oz pigments. The brown, red, and yellow pigments were used interchangeably to vary skin colors. Materials from Reynolds Advanced Material were priced from: https://www.reynoldsam.com/product-category. bPrices obtained from Walmart.com were the Great Value Brand and the lowest price available.
Process
This process outlines the creation of a single pad at a time. These can be multiplied when multiple escargot trays are available simultaneously; however, we recommend not working with more than 3-4 trays at one time, especially until the techniques are mastered. Silicone comes in two parts, A & B, which, once mixed, begin to cure into the desired texture of silicone. These parts need to be kept separate until ready to mix, pour, and mold. The manufacturer lists two times for each type of silicone. Pot time is the amount of time to work with the fully mixed material before it starts to become sticky marking the beginning of curing. Cure time is the time needed to achieve final texture and firmness. Both vary with each product line. Some product lines have multiple pot and cure times. Be aware of these before mixing.
General Silicone Mixing and Pouring
- Pour parts A & B in equal quantities into separate cups, filling each cup no more than halfway.
- If using pigment, mix a small quantity, about a single drop, into Part B. Start with a little, adding more until the desired color is achieved. Mix until uniformly distributed.
- Pour Part A into Part B, scraping the sides to extract as possible. Mix well until color is well distributed, keeping in mind pot times as discussed above.
- When creating layers, we recommend pouring the successive layer before the cure time has completed for the prior layer, but after the first layer has become sticky or about half of the cure time has passed. This will be something to get a feel for over time.
Abscess Pad Process
- Using the modeling clay, form 6 discs about the diameter of the escargot tray well and about as deep as the tray. They should be arched on one side like the curve of the well of the tray. These will be space holders for the simulated pus. Set aside.
- Following manufacturer guidelines, thoroughly and quickly mix approximately 15 ml each (1:1 ratio) of Dragon Skin™ with selected pigment (Silc Pig™) to create a customized skin color. Dragon Skin™ Very Fast pot time is four minutes, and cure time is about 30 minutes (Reynolds Advanced Materials, n.d.).
- Pour the mixture uniformly throughout the 6-well escargot tray.
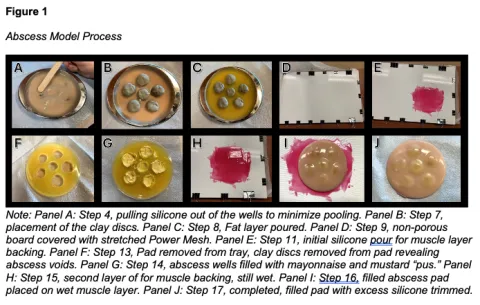
- As the silicone begins to pool in the wells, use a chip brush or similar tool to minimize pooling in the wells while making sure a layer of silicone remains in the wells. The wells will form the wheal of the dermal abscess (Figure 1A).
- Pull some silicone up the sides of the inner walls of the tray for uniform edges of the pad.
- While allowing the silicone to partially cure for about 15 minutes, prepare the fat layer. Mix 30-40 ml each of Ecoflex™ Gel Part A & B with a few drops of yellow pigment to replicate the yellow appearance of body fat until uniformly colored. There is plenty of time to work with this product.
- Place clay discs into the center of each well to form the cavity for simulated pus. Ensure the discs are centered and pressed lightly into the semi-cured silicone (Figure 1B).
- Pour mixed Ecoflex™ Gel into the tray over the silicone and around the clay. The gel does not have to cover the discs but can if necessary to fill to near the top of the escargot tray. Let the gel fully cure (Figure 1C).
- Meanwhile, stretch a sheet of Power Mesh over a flat, non-porous surface (Figure 1D).
- Mix 15 ml each of Part A & B of either Dragon Skin™ or Ecoflex™ 00-30 with a few drops of red pigment to replicate the muscle layer until uniformly colored. Pigmenting the muscle layer is not likely to reduce the product fidelity.
- Spread a thin, even layer of this mixture onto the mesh, ensuring the silicone is pushed through the holes in the mesh. Allow it to cure completely (Figure 1E).
- Remove the cured silicone pads from the tray.
- Extract the clay discs to reveal the internal voids (Figure 1F).
- Fill each void with a mixture of mayonnaise and mustard to simulate pus (Figure 1G).
- Repeat step 10 to create a second red layer. Spread this across the cured red layer poured in Step 11 (Figure 1H). This layer will bond the pad to the bottom layer and seal the filled abscesses.
- Flip each filled pad upside down and press it onto the second, red-pigmented silicone layer while it is still wet, allowing it to attach. This forms the muscle layer. Let this cure thoroughly. (Figure 1I).
- Once fully cured, cut the pad free from the flat surface and remove any excess silicone for clean edges (Figure 1J).
Pilot Testing and Model Implementation for Participants
This project was approved as no more than minimal risk to participants by the University of Central Florida’s IRB, number STUDY00007657 with modification approval number MOD00006599. This study was conducted at the University of Central Florida College of Medicine Clinical Skills and Simulation Center and the Osceola Medical Center. Twenty-two learners voluntarily and anonymously consented to participate in the survey following use of the abscess I&D procedural task trainer. Learners consisted of fourth-year medical students and first, second, and third-year emergency medicine residents during regularly scheduled simulation training. Six participants never performed the skill prior to this training, ten participants indicated they have done the skill at least once but less than ten times, and six indicated they had performed this skill more than 10 times. Learners were required to practice the skill; however, they were not required to complete the survey.
Survey Development and Data Collection
Participants were selected through a convenience sample. The survey consisted of 10 total questions across four different categories. Questions 1-6 evaluated six key aspects of the trainer’s realism using a Likert-type scale from 1 (highly unrealistic) to 5 (highly realistic). Questions 7-8 evaluated the learners’ comfort levels doing the procedure before and after using the trainer using a Likert-type scale from 1 (highly uncomfortable) to 5 (highly comfortable). Question 9 evaluated how likely learners would be to recommend use of the trainer in the future using a Likert type scale from 1 (highly unlikely) to 5 (highly likely). Question 10 was an open-ended response, allowing learners to provide comments. The data was summarized, and statistical analyses were done in Microsoft Excel.
Results
The mean scores and standard deviations of the survey are presented in Table 2. Based on responses to all six realism items, learners rated the trainer’s fidelity as realistic (mean = 4.44, SD = 0.94). The learners’ average comfort level increased significantly by an average of 0.73 (95% CI = 0.31 – 1.14), rising from an average of 3.90 before practicing to 4.60 after using the model. The learners overwhelmingly recommended continued use of this trainer (mean = 4.6, SD = 0.88). After removing one outlier, the mean fidelity rating was 4.56 (SD = 0.65) for participants without prior experience and 4.60 (SD = 0.60) for those who had performed a real abscess I&D, with no significant difference at p = 0.05. Comments generally praised the trainer, complementing its realism and effectiveness as a teaching tool with commenters saying the trainer was particularly useful for training medical students and was helpful for reviewing and practicing the procedure. One commenter suggested using more pus in each abscess.
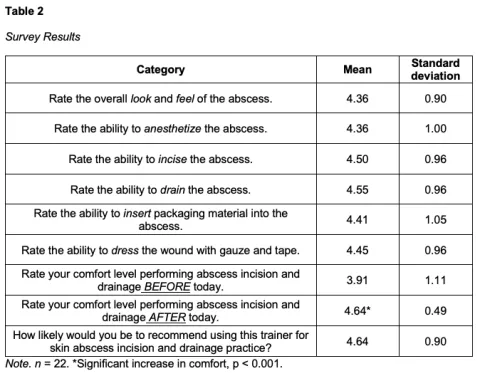
Discussion
This trainer can be constructed quickly with customizable skin tones by personnel with no experience working with silicone. It provides six purulent sites per trainer, allowing for repeated practice and scaling for larger training programs. It is inexpensive with consumable materials costing approximately $7 per pad with six independent abscesses, or a little over $1 per abscess. Based on feedback from medical students and emergency medicine residents, the trainer effectively replicates critical components of abscess I&D including anesthetization, incision, pus expression and drainage, packing, and dressing. The survey results indicate that users were satisfied with all aspects of realism incorporated into the trainer.
Overall, the mean ratings for fidelity-related questions indicated that participants perceived the trainer as highly realistic. Since each area was evaluated independently, this suggests that transitioning from one step of the skill to the next was smooth and replicated a real experience. Participants who had experience incising and draining real abscesses found the overall realism of the trainer to be high (mean = 4.60, SD = 0.60). This indicates that those who had experience incising and draining real abscesses found this trainer to be close to their experienced reality, further attesting to the procedural fidelity of the trainer.
In addition, two anomalies were identified in the survey results. One participant rated the fidelity of all procedural steps realistic or highly realistic; however, they indicated they were highly unlikely to recommend using this trainer. Another participant rated almost all the step fidelities as highly unrealistic; however, they were highly likely to recommend using this trainer. This represents a potential limitation in the data. Since there were only 22 participants who self-selected into the study, participation bias exists, and outliers can have a greater impact on overall averages and standard deviation.
Limitations and Opportunities for Future Research
There were several limitations to this study. To begin with, the sample size of learners was small and therefore could limit the generalizability of the results. Further research would be needed to evaluate if the results presented here are replicated in other groups. Only medical students and residents participated in the study. Providers who perform the skill frequently such as attending physicians, family nurse practitioners, and physician associates, among others, may have a different assessment of this trainer. Future studies including experienced providers is warranted.
The survey was conducted via a convenience sample, introducing potential for selection bias in participants. However, there was not a pre-test/post-test survey design to accurately capture participants anxiety, comfort, or competence with abscess I&D before and after using the trainer. Although these data indicate a significant improvement in comfort after using this trainer, more research would help further understand the benefits of the trainer, especially in novice learners.
The residents were all emergency medicine residents from a single residency program. Future participants should include residents from other specialties who are likely to need experience with abscess I&D. Additionally, the medical students included happened to be rotating in emergency medicine during the time of the skills training. Evaluating a broader swath of medical students would further enhance the generalizability of the study. This trainer would benefit from input from additional providers including physician assistants, family nurse practitioners, dermatologists, and emergency medicine physicians.
Another future research consideration would be to directly compare the fidelity and learner preference of this trainer to other trainers, including both commercial and homemade models. Although this trainer addresses several issues present in other models, this study cannot conclude that it is superior to trainers reported in the literature or available commercially.
Conclusion
Our innovative, low-cost skin abscess incision and drainage procedural task trainer created from silicone cast in an escargot tray mold was viewed as realistic in its procedural steps by medical students and residents. Simultaneously, the trainer shows distinct promise as a model which overcomes the various shortcomings present in other homemade and commercial models, including cost, perishability, and limited ability to perform all steps in the I&D procedure. The trainer was perceived as allowing realistic practice of anesthetizing, incising, draining, packing, and dressing a skin abscess. Learners increased their comfort in performing the skill in the clinical environment and encourage continued use of this model for future trainings.
References
Chambers, O., Eckhardt, D., & Jackson, T. (2024). Development of a Novel, Reusable Task Trainer for Foreign Body Removal and Abscess Incision and Drainage. The Journal of Physician Assistant Education, 35(3), 237–242. https://doi.org/10.1097/JPA.0000000000000580
Done, A. J., Fairres, M. J., & Heiler, J. C. (2020). A low-cost high fidelity model for abscess simulation. The American Journal of Surgery, 219(4), 628–631. https://doi.org/10.1016/j.amjsurg.2019.06.011
Gordon, C. J., Ryall, T., & Judd, B. (2016). Simulation-based assessments in health professional education: A systematic review. Journal of Multidisciplinary Healthcare, 69. https://doi.org/10.2147/JMDH.S92695
Heiner, J. D. (2010). A New Simulation Model for Skin Abscess Identification and Management. Simulation in Healthcare, 5(4), 238–241. https://doi.org/10.1097/SIH.0b013e3181d87f0f
Nicka, A., & Swanson-Biearman, B. (2019). Development of a Subcutaneous Abscess Simulator for Incision and Drainage. Clinical Simulation in Nursing, 37, 40–43. https://doi.org/10.1016/j.ecns.2019.08.001
Pastorino, A., & Tavarez, M. M. (2024). Incision and Drainage. In StatPearls. StatPearls Publishing.
Reynolds Advanced Materials. (n.d.). Retrieved August 7, 2025, from https://www.reynoldsam.com/?srsltid=AfmBOor_aui5lKmTLimEhWcdz3hmja1iP76akY Baw3uHmlCFoF_-wJ9s
Sagalowsky, S. T., Wynter, S.-A., & Auerbach, M. (2016). Simulation-Based Procedural Skills Training in Pediatric Emergency Medicine. Clinical Pediatric Emergency Medicine, 17(3), 169–178. https://doi.org/10.1016/j.cpem.2016.05.007
Singh, M., & Restivo, A. (2024). Task Trainers in Procedural Skills Acquisition in Medical Simulation. In StatPearls. StatPearls Publishing.
Thyagarajan, M., Sundaramoorthy, E., & Nallasivam, M. (2024). Novel indigenous low cost (NICA) model for hands on training of surgical interns in incision and drainage procedure for superficial skin abscess. BMC Medical Education, 24(1), 1386. https://doi.org/10.1186/s12909-02406013-w