Authors
Sharon R. Stiles, MBA1, Tara L. Petersen, MD, MSEd1,2, Lucia G. Lee, MS1, Katie L. McDermott, PhD, MEHP, RN, CPNP-AC1, 2, 3
1Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI
2Dairy Cares of Wisconsin Simulation Lab, Children’s Wisconsin, Milwaukee, WI
3College of Nursing, Marquette University, Milwaukee, WI
Conflict of Interest Statement
This project received no sources of funding. The authors report no conflicts of interest.
Corresponding Author
Sharon R. Stiles, MBA, Medical College of Wisconsin, Department of Pediatrics, Milwaukee, WI
(Email: sstiles@mcw.edu)
Abstract
Introduction: Simulation event scheduling is a key operational aspect of planning and executing simulation-based education events. This hospital-based simulation center identified the need for a more efficient, functional, and forward-facing scheduling process to ease the workload of program staff and increase the satisfaction of facilitators and users.
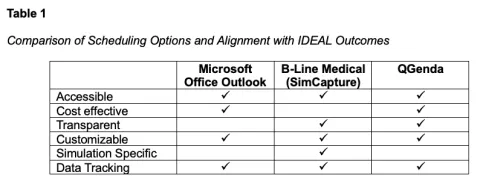
Methods: The IDEAL Problem-Solving Model was used to organize the project, systematically explore available scheduling options, and generate a creative and informed solution. The three options considered were: Microsoft Office Outlook, B-Line Medical (now SimCapture), and QGenda. Each option was evaluated based on simulation center priorities, including accessibility, cost-effectiveness, transparency, customizability, simulation specific, and ability to track data.
Results: This simulation center selected QGenda as the best scheduling platform option. QGenda is a hospital-based platform used for healthcare workforce management. It was already in use within the hospital system and was adapted for simulation center scheduling processes. The introduction of QGenda as the scheduling platform yielded process and operational improvements, including decreased emails, more timely event scheduling, staff and user satisfaction, and event tracking with reports generated using data management functionality.
Conclusions: QGenda has proven to be an inspired and functional option as a simulation scheduling platform. Especially for hospital-based simulation centers that already utilize QGenda for clinical-based and workforce scheduling, extending its use to simulation scheduling can be cost-effective and may result in little to no additional cost to the program.
Introduction
Scheduling is an important part of planning and executing simulation-based education events (Dongilli et al., 2015). Scheduling processes involve a variety of components, including reservation of time, space, personnel, and equipment, as well as administrative logistical coordination of approvals and assurance of resource availability across multiple events (INACSL Standards Committee et al., 2021). Ineffective scheduling increases user frustration, minimizes use of simulation space, and increases programmatic costs. Moreover, many simulation centers are located within institutions such as hospitals or universities, requiring scheduling systems that can be accessed and integrated with other institution-specific systems.
Several scheduling platforms are available; however, they can be difficult to tailor to the unique needs of individual simulation programs. Similarly, many scheduling platforms come at a high cost, are incompatible with other programs, and may be inaccessible to all users in multi-organizational simulation centers. Microsoft Office Outlook and Learning Management Systems have been used by simulation centers for scheduling (Grant et al., 2020; Wood et al., 2014). Microsoft Office Outlook can be a cost-effective scheduling system, but only if all users have access to and enable bidirectional calendar viewing (Grant et al., 2020; Wood et al., 2014). Many institutions have existing platforms available to employees for trainings and meeting space reservations. Although these platforms have scheduling operations, they are not specific to simulation scheduling, are purchased through external vendors, require additional orientation, or involve lengthy processes and costs to approve new uses or new vendors (Grant et al., 2020). This project aimed to identify and implement a transparent, easily accessible, customizable, cost-effective, and simulation specific scheduling platform for this hospital-based simulation center.
Methods
To address the issues surrounding simulation center scheduling processes, the IDEAL Problem-Solving Model was used to generate creative solutions and to organize and implement the project (Bransford et al., 1998; Bransford & Stein, 1984). The IDEAL model consists of the following steps: 1) Identify the problem, 2) Define the outcomes, 3) Explore possible strategies, 4) Anticipate outcomes and act, and 5) Look back and learn. This simulation center is located within a free-standing, quaternary care academic children’s hospital in the Midwest United States. It contains five high-fidelity simulation rooms, one debriefing room, one exam room, one virtual reality room, one classroom, one conference room, and one flexible space dedicated to skills and procedures. The simulation center hosts a variety of event types, ranging from individual just-in-time training sessions to large-scale multi-institutional simulation workshops. It serves multidisciplinary participants at all levels of training with an average of 11,000 annual learner contact hours.
Results
Identify the Problem
The first step of the IDEAL model was to identify the problem: the lack of an efficient simulation scheduling process. Prior scheduling processes consisted of primarily unstructured email communication between an event facilitator and a simulation program staff member to query availability for a specific day and time. Frequently, back-and-forth messaging was required to successfully schedule a date, time, space, and equipment for each event. The event date and time was then manually entered by the staff member into the simulation center’s Outlook calendar, only viewable to program staff due to institutional restrictions and associated firewalls. On average, four emails over a duration of twenty days were required to successfully schedule the various components of a simulation event. This resulted in cumbersome communication, limited transparency of facilitator availability, and increased risk of transcription errors.
Define the Outcomes
The second step of the IDEAL model was to define the outcomes in order to address the problem and inform possible solutions. The first outcome was to provide a scheduling process with well-defined procedures that were easily accessible, cost-effective, transparent, customizable, and simulation specific. The second outcome was to incorporate the ability to efficiently document, track, and report event data, such as number of events, total education time, and participant demographics. This outcome was considered important by staff, program leadership, and other key stakeholders, as it provided data-driven insights into resource use and event trends, supporting future strategic planning for program expansion and development.
Explore possible strategies
With the problem and outcomes defined, the third IDEAL step was to brainstorm all possible strategies. Simulation program staff and leaders engaged in thoughtful dialogue and consulted a variety of key stakeholders, including corporate hospital sponsors, academic medical program leadership, funding groups, event facilitators, and participants to ensure the solutions addressed the spectrum of scheduling needs. Several simulation-specific and non-simulation-specific scheduling options were identified. The strengths and weaknesses of each option were evaluated based on the identified outcomes. Scheduling options explored were Microsoft Office Outlook (Microsoft, 2025), B-Line Medical/SimCapture (Laerdal Medical, 2024), and QGenda (QGenda, LLC, 2024).
Microsoft Office Outlook is a non-simulation email and calendar platform used by many institutions. Given it is already widely accessible and used institution-wide, it is considered cost-effective and may result in no direct costs to the simulation program. Microsoft Office Outlook contains embedded and customizable scheduling features which allow users to schedule rooms for a specific date and time and generate reports for event tracking. Users can choose to share either individual calendar events or an entire transparent shared calendar, with some notable limitations. Many times, users do not have the option to share calendars across different employers and/or institutions, limiting usability. As a result, when users view the calendar, the platform may not accurately display room availability if used across multiple institutions, limiting transparency for end-users.
B-Line Medical/SimCapture is a simulation-specific scheduling platform which allows a center to customize scheduling options based on the number of simulation spaces and many other variables. This platform also provides transparent availability between the program and users. The schedule is viewable by users with a B-Line Medical/SimCapture account; however, most employees and end-users do not have an account, which limits schedule accessibility. Additionally, B-Line provides data storage of event details that can be exported for data tracking. Despite these strengths, B-Line Medical requires a significant investment of time for platform management, as well as both upfront and ongoing costs for subscribing to the specific modules needed by the program.
The third option considered was QGenda, a scheduling platform used by healthcare organizations for healthcare workforce management. Although it is not simulation-specific, it can be customized with names of simulation rooms and provide transparency into room availability. Similar to Microsoft Office Outlook, many institutions already use QGenda system-wide; therefore, users already have access, and it requires no additional direct financial investment from the simulation center. It has capacity for data collection and extraction for simulation event tracking. Finally, QGenda has the unique feature of synchronizing with Microsoft Office Outlook calendars across different institutions, eliminating the need for manual event entry. In turn, this has the potential to save staff time and minimize the risk of transcription errors.
After thoughtful review of the three possible solutions, QGenda was selected as the best option because it most closely aligned with the program’s defined outcomes (Table 1). As the hospital was already using QGenda as a scheduling platform, existing infrastructure was already in place to support the adoption of this platform. The supportive infrastructure included easy access to the QGenda application through the hospital’s main internal website, IT expertise, and hospital employees’ existing familiarity with the platform.
To begin the transition to QGenda as the simulation center’s scheduling platform, staff met with a QGenda representative and discussed logistics and timeline for implementation. QGenda was customized to incorporate all simulation center rooms and spaces, which were then displayed to users as either “booked” or “available” for the date and time of interest. This created a forward-facing schedule for all users by allowing users to see if their desired room, date and time were available, while also showing alternative available options. Program staff had administrative access to adjust the availability of each room and space (Figure 1). Finally, QGenda representative support is not required on an ongoing basis, only for the initial build of the simulation center schedule or in the event of major changes, such as adding new spaces or changing room names.
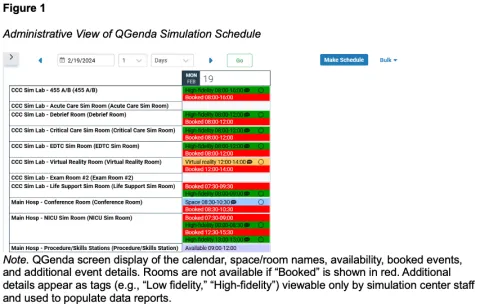
Note. QGenda screen display of the calendar, space/room names, availability, booked events, and additional event details. Rooms are not available if “Booked” is shown in red. Additional details appear as tags (e.g., “Low fidelity,” “High-fidelity”) viewable only by simulation center staff and used to populate data reports.
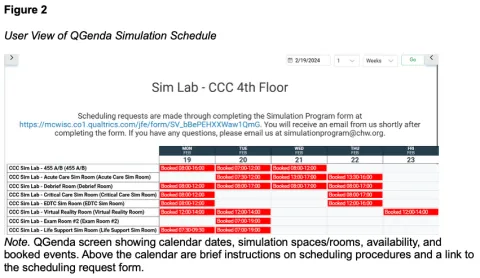
Part of the first outcome was to provide an easily accessible scheduling platform across the institution. To address this, the simulation schedule was added to the institution’s internal webpage. The webpage was already the designated location to access QGenda for other programs and was therefore familiar to users. It is available to any person working or training within the hospital, regardless of employer, eliminating the need for additional logins or specific access permissions. Users can apply filters to view specific simulation areas during their desired timeframe. To further augment accessibility and usability, instructions and related external links, such as the simulation program’s reservation form and contact information, are located on the simulation center QGenda page (Figure 2).
This simulation center is located in a hospital which was already invested in and using QGenda for healthcare workforce management. Therefore, there were no upfront or direct costs to the simulation program to implement QGenda. Additionally, there were no associated maintenance or simulation-specific subscription costs, such as those with the B-Line Medical platform.
Finally, QGenda contained features for documenting, tracking, and reporting simulation event data. It allowed simulation staff administrative access to scheduling and event data, including categorization of event types (e.g., high-fidelity, low-fidelity, space), frequency of use of rooms/spaces, and trends in frequency of use (e.g., days of the week, times of the day).
Anticipate outcomes and act
The fourth step of the IDEAL model was to anticipate outcomes and act. This step involved expecting a range of reactions, planning how to navigate them, and considering sustainability and future state of the solution. With any change comes a variety of responses, both positive and negative (Harrison et al., 2021). Simulation event facilitators expressed satisfaction with the ability to easily view room availability. This allowed self-selection of an available date and time on the front end of the scheduling process and eliminated the need for multiple emails. Many simulation center users were already familiar with QGenda as part of their clinical workflow; therefore, issues related to learning a new and unfamiliar system were minimized. To mitigate perceived barriers by individuals not previously familiar with QGenda, program staff provided tutorials regarding how to find the calendar on the internal website and navigate the various features.
One future consideration is the impact on the simulation center if the hospital decides to transition from QGenda to a different workforce management system. Currently, QGenda is highly utilized and integrated across the system; therefore, an intensive process would be required to select and implement any new system for this purpose. If this were to occur, the simulation center would undertake a similar process described here to identify a scheduling platform. Simulation staff and leadership overwhelmingly felt the benefits of adopting QGenda for simulation scheduling outweighed the possible and hypothetical risks of eventually losing access and having to again find a new platform.
Look back and learn
The final step in the IDEAL model is to look back and learn to reflect upon success and identify further areas of opportunity. The overall timeline of the project was six months, from problem identification to fully functional QGenda implementation. Once QGenda was selected as the scheduling solution, simulation staff and QGenda representatives collaborated to customize the platform and define scheduling procedures. Prior to the institutional QGenda go-live, a one-month pilot was conducted wherein select simulation center users accessed QGenda to schedule their events and provided feedback on the platform and scheduling process. Email communication was sent to frequent simulation center users to announce the transition to QGenda and provide instructions regarding access and procedures. Additional users were informed and trained on a rolling basis. Supplemental resources regarding QGenda orientation and related scheduling procedures were created, including a detailed how-to guide with screenshots and links. This was available to users via email and posted on the simulation center intranet site. Simulation staff were also available to provide direct assistance and answer questions.
QGenda was an inspired solution to the large problem of scheduling for the simulation center. It successfully addressed the programmatic goals of being easily accessible, cost effective, transparent, customizable, and allowing for data management. All limitations to the platform were anticipated regarding how people would navigate and accept a change in scheduling procedures. Constructive feedback from users was acknowledged and quickly resolved with just-in-time education, as well as thoughtful, timely, and efficient responsiveness from simulation staff to address issues as they arose.
Discussion
The QGenda scheduling solution was introduced within this simulation center in August 2021 and remains the current scheduling platform. Since that time, 2,217 events and 7,651 event hours were scheduled (August 2021 to December 2024) using QGenda. Prior to the implementation of QGenda, an average of four emails over a duration of twenty days was required to schedule an event, whereas now an event is scheduled after one confirmation email within two business days. Most of the time, the user can view the transparent schedule, submit a request, and receive a one-time email confirmation of their request without further communication. Additionally, program staff can synchronize QGenda with Microsoft Office Outlook calendars to eliminate the need for manual entry and associated transcription errors.
Users had the opportunity to share feedback regarding the scheduling process by using the program’s optional anonymous feedback survey. One hundred percent (n = 21) of survey participants rated the ability to view simulation space availability within QGenda as useful and helpful. Additionally, in the free text response option, participants stated it was “very easy to identify open times the simulation area was available for our use with the current scheduling methods,” “much improved from previous scheduling abilities,” and that the “scheduling process is very organized”.
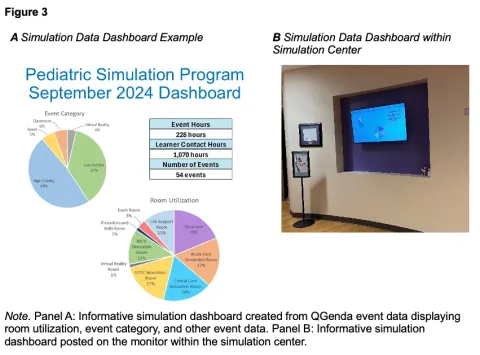
Finally, the use of QGenda to collect, organize, and report event trends has facilitated a data-driven approach to decision-making regarding simulation program development, such as equipment purchases, space allocation, and staffing requirements. Data reports can be generated and used to create informative dashboards to display user statistics, such as space, education hours, learner contact hours, and event types (Figure 3A). The data and dashboards are used in a variety of ways to demonstrate the impact of simulation, such as the generation of business plans, crafting annual reports, and demonstrating the use of philanthropic donor funds. Additionally, the dashboards are publicly displayed on a large monitor upon entrance to the simulation center, which increases awareness and highlights the various simulation events across the institution (Figure 3B).
Conclusion
Scheduling is a vital aspect of the daily operations and management of a busy simulation center. QGenda is a cost-effective scheduling system, especially for simulation centers affiliated with a healthcare or hospital-system that is already using it for workforce management. This platform benefits users by being easily accessible and transparent, with the ability to efficiently view availability and schedule a simulation event. QGenda benefits simulation program staff and leaders through its functionality as a data management system to facilitate data-driven decisions and informed strategic planning.
References
Bransford J.D., Haynes A.F., Stein B.S., Lin X. (1998). The IDEAL workplace: Strategies for improving learning, problem solving, and creativity. (pp 1-5). Nashville, TN, NashvilleREAD.
Bransford, J. D., & Stein, B. S. (1984). The ideal problem solver. A guide for improving thinking, learning, and creativity. In W.H. Freeman eBooks. http://ci.nii.ac.jp/ncid/BA44989141.
Dongilli, T. A., Shekhter, I., & Gavilanes, J. S. (2015). Policies and procedure. In J. C. Palaganas, J. C. Maxworthy, C. A. Epps, & M. E. Mancini (Eds.), Defining excellence in simulation programs (pp. 354–363). Lippincott Williams & Wilkins.
Grant, V. J., Catena, H., & Peiris, N. (2020). Simulation operations. In M. Seropian, G. Keeler, & V. Naik (Eds.), Comprehensive healthcare simulation: Program & center development (p. 102). Cham, Switzerland, Springer Nature Switzerland.
Harrison, R., Fischer, S., Walpola, R. L., Chauhan, A., Babalola, T., Mears, S., & Le-Dao, H. (2021). Where do models for change management, improvement and implementation meet?: A systematic review of the applications of change management models in healthcare. Journal of Healthcare Leadership, 13, 85–108. https://doi.org/10.2147/JHL.S289176.
International Nursing Association of Clinical Simulation and Learning [INACSL] Standards Committee, Charnetski, M., & Jarvill, M. (2021). Healthcare Simulation Standards of Best Practice® Operations. Clinical Simulation in Nursing, 58, 33-39. https://doi.org/10.1016/j.ecns.2021.08.012.
Laerdal Medical. (2024, July 2024). SimCapture – Manage simulation trainings and exams. https://laerdal.com/information/simcapture-solution-features.
Microsoft. (2025). Microsoft Support: What is Outlook? Microsoft Office. Retrieved July 23, 2024, from https://support.microsoft.com/en-us/office/what-is-outlook-10f1fa35-f33a-4cb7-838c-a7f3e6228b20.
QGenda, LLC. (2024, December 17). Healthcare Workforce Management Solutions - QGENDA. https://www.qgenda.com/.
Wood, J. L., Whitman, B. J., Mackley, L. A., Armstrong, R., & Shotto, R. T. (2014). A customizable, scalable scheduling and reporting system. Simulation in Healthcare, 9(3), 192–198. https://doi.org/10.1097/SIH.0000000000000020.